More than 130000 clariVein® units are in market*. The clariVein® device is designed to benefit patients and physicians alike.
The clariVein®OC is a specialty infusion catheter with a rotating wire tip designed for the controlled 360-degree dispersion of physician-specified agents to the targeted treatment area. Often referred to as MOCA (mechanical occlusion chemically assisted), the ClariVein®OC Device offers many unique and proven benefits:
- Non-tumescent
- Reduced Pain1
- Non-thermal
- Reduced Recovery Time1
- Clinically Proven
- Reduced Procedure Time1
clariVein®OC Advantage
ADVANTAGES
Physician
Patient
MINIMALLY INVASIVE^
FAST PROCEDURE TIME^
QUICK RETURN TO NORMAL ACTIVITIES^
minimizes patient discomfort^
PERFORMED IN AN OFFICE SETTING^
tumescentless procedure decreases procedure time^
SELF-CONTAINED DISPOSABLE DEVICE
reduced cost: no user servicable parts
^ Data on file
1. R. van eekeren, et al., Postoperative Pain and Early Quality of Life After Radiofrequency Ablation and Mechanochemical Endovenous Ablation of Incompetent Great Saphenous Veins, journal of vascular surgery, Volume 57, Number 2, February 2013, p. 445-450.
clariVein®OC Comparison to Thermal Ablation
clariVein
Thermal Ablation
requires tumescent anesthesia
Thermal Ablation –Yes
clariVein –No
Risk of Thermal Damage
Nerves, Skin, Paresthesia
Thermal Ablation –Yes
clariVein –No
Percutaneous Access
Thermal Ablation –6 F or Larger
clariVein –4 F or Larger
Thermal Ablation –Yes
clariVein –No
Lease Agreement
Thermal Ablation –Yes
clariVein –No
Contract Purchasing
Thermal Ablation –Yes
clariVein –No
Equipment Maintenance Contract
Thermal Ablation –Yes
clariVein –No
Treatment Suitability
Thermal Ablation – & SSV
-May not be suited for smaller vessels due to thermal damage risk 1
clariVein –GSV & SSV
-Plus small vessels all the way to ankle. Some studies show success in the venous ulcer beds2
Patient Pain & Bruising
Thermal Ablation –Risk from thermal energy 2
clariVein –74% less post-operative pain1
less bruising
Vascular Imaging
Thermal Ablation –Yes
clariVein –Yes
positioning technique
Thermal Ablation –2 cm from SFJ
clariVein –2 cm from SFJ
Pullback Timing & Method
Thermal Ablation –RF: park and Wait
LASER: 1.5mm/second
clariVein –1-3mm/second
^ Data on file
1. R. van eekeren, et al., Postoperative Pain and Early Quality of Life After Radiofrequency Ablation and Mechanochemical Endovenous Ablation of Incompetent Great Saphenous Veins, journal of vascular surgery, Volume 57, Number 2, February 2013, p. 445-450.
2. Hayley M Moore, Tristan RA Lane, Ian J franklin and alun H davies Retrograde Mechanochemical Ablation of the Small Saphenous Vein for the Treatment of a Venous Ulcer 1708538113516320 first published December 17, 2013
clariVein®OC Versus Radiofrequency
Postoperative pain and early quality of life after radiofrequency ablation and mechanochemical endovenous ablation of incompetent great saphenous veins 1
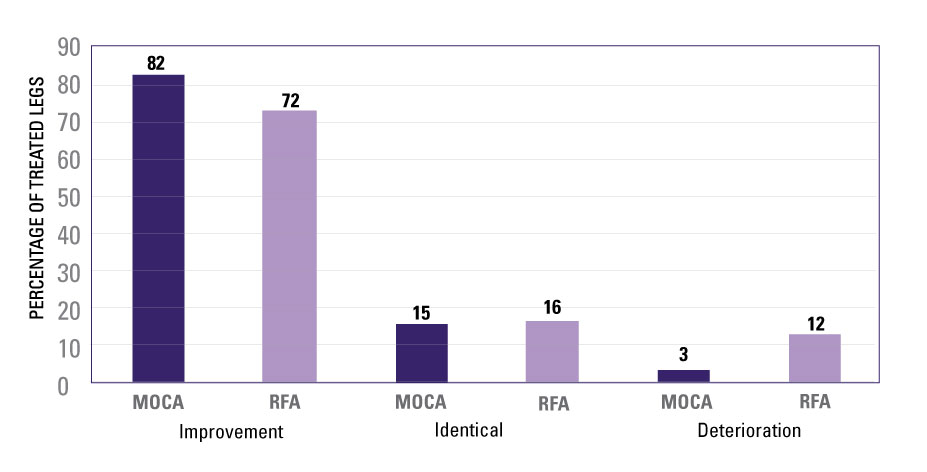
Fig 1. Assesment of the Venous Clinical Severity Score (VCSS) 6 weeks after the treatment with mechanochemical endovenous ablation (MOCA) and radiofrequency ablation (RFA).
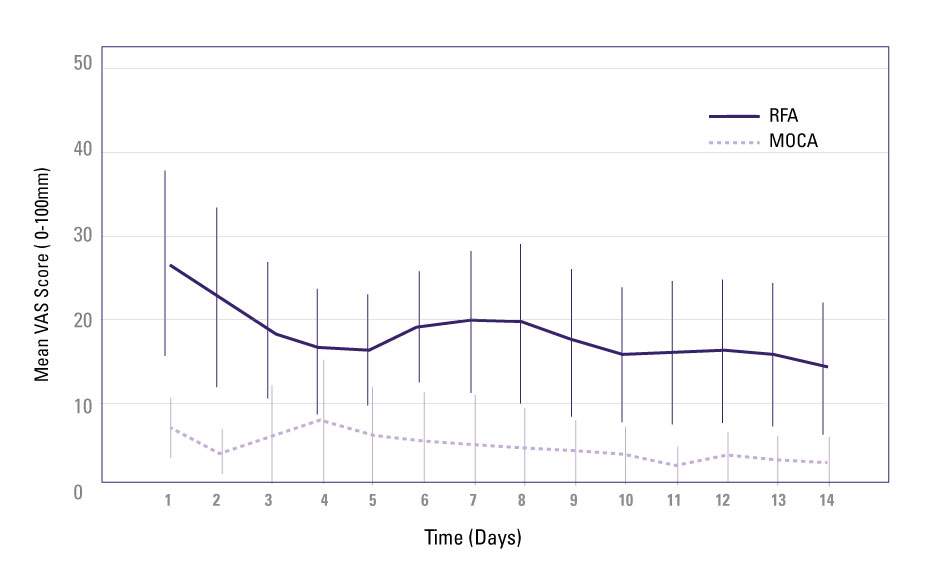
Fig 2. Mean postoperative pain scores on a 0 to 100 mm visual analogue scale for 14 days after mechanochemical endovenous ablation (MOCA) and radiofrequency ablation (RFA). CI, Confidence interval; VAS, visual analog scale.
- “This study has demonstrated that postoperative pain is significantly lower after MOCA compared with RFA, corresponding to a 74% reduction in pain for the first 14 postoperative days.”
- “The time to return to normal activities was 1.0 day (IQR, 0-1.0) in the MOCA group and 1.0 day (IQR, 1.0-3.0) in the RFA group, which was significantly longer (P=.01).”
- “The median time to work resumption for employees was significantly shorter in the MOCA group than in the RFA group (P=.02), respectively, 1.0 days (IQR, 1.0-3.75) vs 2.0 days (IQR, 2.0-7.0).”
^ Data on file
1. R. van Eekeren, et al., Postoperative Pain and Early Quality of Life After Radiofrequency Ablation and Mechanochemical Endovenous Ablation of Incompetent Great Saphenous Veins, Journal of Vascular Surgery, Volume 57, Number 2, February 2013, p. 445-450.